Chiropractic SOAP note software is more important than ever with the recent introduction of ICD-10 codes. It’s a fact that chiropractors will be judged more critically now on documentation in the new ICD-10 era. Your daily SOAP notes must be detailed enough to support the use of the new codes if you expect to be reimbursed for your services. This is especially true when trying to meet Medicare chiropractic documentation guidelines.
ICD-10 Impact on Chiropractic SOAP Notes
One of the primary reasons that ICD-10 codes have been implemented is for greater accuracy compared to the previous ICD-9 code set. While this is an admirable goal, the backlash is that your documentation will also need to reflect that specificity. It’s no longer enough to document whether a muscle strain exists, you must also document the specific laterality, muscle, and/or anatomical location, as well as specific objective findings that help to support the diagnosis. If your daily SOAP notes do not contain the required level of specificity to support the codes being used, then you risk being denied payment for your services by insurance payers.
Chiropractic SOAP Note Software Can Help With Compliance
As you can see, documenting to this level of specificity can become quite cumbersome if you are still documenting your notes by hand. Chiropractic SOAP note software can help you to automate this process, ultimately saving you time and improving your chances of being reimbursed for your services.
One misconception a lot of chiropractic professionals have is that a software exists that will auto-generate the perfect SOAP note that will be invincible from all documentation denials or audits. This couldn’t be further from the truth. That’s like expecting a piano to produce the perfect melody, regardless of the musician’s skill level. As the saying goes, garbage in, garbage out.
Essential Components of SOAP Notes for Chiropractors
Before you can understand or appreciate how software can improve your SOAP notes, you first need to understand the reasons we document our patient encounters in the first place. Your daily notes are the chronological record of your patient’s presentation, treatment and response to care. They also help to justify your treatment and charges in the event of an audit and can protect you against a malpractice suit.
SOAP is a simple mnemonic, which stands for Subjective, Objective, Assessment and Plan.
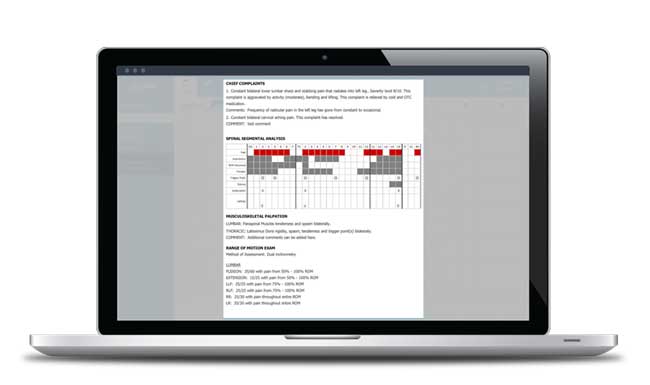
Subjective: This covers the patient history, including the review of intake forms. Anything the patient reveals about their complaint belongs in this section.
Objective: This is your record of the physical examination portion of the patient encounter, including the results of any laboratory and imaging tests that may be performed.
Assessment: This is your diagnosis, as well as your assessment of progress.
Plan: This is your plan of care. It includes not only your initial treatment plan (expected duration and frequency of care along with recommended services, including any possible additional testing, etc.) but on subsequent visits, the treatment rendered on that encounter, home recommendations, referrals to other providers, etc. It should also include the patient’s response to the treatment (i.e., patient tolerated manipulation well and reports pain has reduced from a 6/10 to a 3/10).
Simple Strategies Chiropractors Can Use To Improve Their SOAP Notes
There are many simple strategies that can be employed by chiropractors to improve and achieve defensible documentation. Here are three of the most common mistakes chiropractors make in their SOAP notes.
Failure to Report Your Patient's Response to Treatment
While this makes for good common sense, few chiropractors document their patient’s response to treatment regularly. So, it is no surprise that third-party payers will use this lack of reporting against us when considering payment. Think about it, they are footing the bill and want to know if the care you are providing is actually helping the patient. The documentation of the response to treatment need not be lengthy or difficult, but it does need to be there in your notes. At its most basic level, this should include reporting that the patient is “same, better or worse” compared to their last adjustment.
Mismatching Objective Findings With Treatment
From a Payer perspective, reimbursement can only be made when medical necessity is proven for the care rendered. What this means on a practical level is that if you adjust the cervical, thoracic and lumbar spine, you’d need to have objective findings to prove the medical necessity of your treatment in these regions if you expect to be paid. When there are no objective findings to match up with your treatment, your claim will either be denied or downcoded. Even if your claim does get paid, you run the risk of failing a potential audit and having to repay the money later.
Poor Legibility of Notes
If your documentation cannot be read, it is considered improperly done. Legible doesn’t mean that you can read your own notes. It means that any reasonable person can read them, whether it be another Provider, insurance adjuster or attorney.
I have yet to come across a chiropractic SOAP note software that wasn’t capable of producing an organized and legible note. If your notes are illegible or confusing to those who read them, do yourself a favor and protect your income. Switch to a chiropractic EMR software that can produce a note you can be proud of. Even if your documentation isn’t perfect, it will be substantially better because it’s legible.
The Dead Doctor Rule
To help gauge if you’ve written a good SOAP note, you should apply the “dead doctor” rule: Ask yourself the question that if you were to die tomorrow, could another doctor with no idea of what’s going on, understand what’s wrong with your patient, where they are in their progress, and so on, after reviewing your notes? That’s a measure of good documentation.
Chiropractic Documentation Software Can Save You Time and Money
The right chiropractic SOAP note software can accelerate the input of pertinent data, and format it in an organized and legible fashion. For most doctors, this can amount to saving a considerable amount of time doing paperwork and reduced denials from Payers. It’s important to remember that it’s ultimately the doctor’s responsibility to accurately report what’s going on and to justify their treatment, not the software’s.